Hiatal hernia, gastroesophageal reflux and their surgical treatment - Dr. Bruto Randone
What is it?
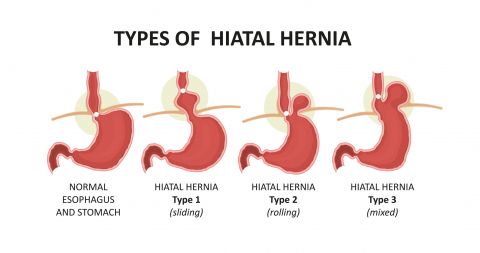
It is an upward displacement of the junction between the esophagus and the stomach (sliding hernia, type 1) or the ascension of part of the stomach only (rolling hernia or paraesophageal hernia type 2), or both conditions together (mixed hernia, type 3).
This movement is carried out from the abdominal side of the diaphragm (dome-shaped muscle, which separates the thorax from the abdomen), towards its thoracic side.
The end portion of the esophagus at its junction with the stomach contains a device called the lower esophageal sphincter. It allows food to pass into the stomach, but at the same time prevents the contents of the latter from flowing back into the esophagus.
When the junction between the stomach and esophagus rises above the diaphragm, the lower esophageal sphincter loses its effectiveness, exposing the patient to the most troublesome complication of hiatal hernia, gastroesophageal reflux disease (GERD).
In this case, gastric acid, which is useful for digestion, can flow back into the esophagus. This is a very powerful acid, which causes irritation and a burning sensation characteristic of reflux.
We have all experienced GERD occasionally, because hiatal hernias are not the only condition that puts one at risk for GERD, but if you suffer from it at least twice a week, for several weeks, it is considered chronic GERD.
The symptoms linked to GERD vary depending on the extent of acid reflux:
Regurgitation: food coming up to the throat, we can sometimes appreciate the bitter taste of gastric acid or notice bad breath.
Pyrosis: this occurs when the acid “burns” the tissues of the esophagus.
Chest pain: sometimes we can appreciate pain that does not feel like a burning sensation. The esophagus can stimulate the same nerves that cause cardiac pain.
Nausea: Acid reflux can cause you to lose your appetite, even if you have eaten a while ago, you may have the feeling that there is still food to digest.
Sensation of a lump in the throat and/or difficulty swallowing: if the acid rises to the throat, it may give the sensation of having something in the throat, or that it is difficult to swallow.
Asthma-like symptoms: if the acid enters the respiratory tract, it can cause them to contract, triggering symptoms such as chronic cough, dyspnea or wheezing.
The most dangerous aspect of long time chronic GERD is the complications caused by the constant attack of gastric acid.
Esophagitis: this is the inflammation of the tissue that covers the inside of the esophagus (mucosa), it can evolve into ulceration and, after some time, it can lead to dysplasia which lead to Barret's esophagus.
Barret's esophagus: Cells in the esophageal lining, to protect themselves from prolonged exposure to acid, can transform to resemble cells in the stomach. This is a pre-cancerous lesion.
Esophageal stricture (stenosis): the inflamed tissue of the esophagus can develop scarring, which narrows the diameter of the esophagus itself. This situation can lead to difficulty eating or drinking.
Dental damage: tooth enamel can be damaged following repeated acid attacks and weaken dental defense mechanisms.
DIAGNOSIS
Tests used to diagnose a hiatal hernia and assess possible reflux are as follows:
Barium swallow test: this involves performing a few x-rays while you ingest a radio-opaque liquid to assess the hiatal hernia and reflux.
Endoscopy: we perform an esophagogastric fibroscopy to view the interior of your esophagus and stomach to detect lesions related to reflux.
Esophageal PH test: this test measures acidic episodes that occur over 24 hours and their correlation with your symptoms.
Esophageal manometry: this test measures the muscular activity of your esophagus, using pressure sensors. It can determine if the lower esophageal sphincter is not doing its job properly.
Treatment
Change in health and diet habits.
If GERD is not chronic, some may benefit from some lifestyle adjustments, such as avoiding foods and beverages that stimulate acid production or reducing alcohol and tobacco consumption or losing weight.
Drugs
When diagnosed, we first opt for medical treatment.
The most frequently used medications are:
Antacids: They neutralize gastric acid and reduce its corrosive effect on the esophagus. But they can have collateral effects, so they are not a long-term solution.
Alginates: They form a physical barrier between the acid and the esophagus.
H2 blockers: They reduce stomach acid production by blocking the molecule that tells our body to produce more acidity (Histamine).
Proton pump inhibitors (PPIs): These are more powerful acidity “blockers” that promote healing at the same time. They are effective in 90% of cases.
It must be said that all these medications treat the symptoms and not the causes of reflux, which will persist even if they are less apparent.
Long-term medical treatment can cause significant side effects, according to some studies. This is the case, most recently with certain studies which have established a correlation between long-term PPIs and dementia.
As if this were not enough, scientific studies have failed to demonstrate that drug treatment can reduce or cancel the risk of cancerous degeneration of the lower part of the esophagus.
The cause of reflux, therefore, can only be treated with surgery.
SURGICAL TREATMENT
Surgeries for hiatal hernia repair are carried out using a minimally invasive technique (laparoscopy) with or without robotic assistance.
As this is a surgery which involves the use of several sutures (between the two pillars of the diaphragm and between the stomach and the esophagus), the use of the robot brings a particular ease to the gestures.
There are several types of surgical techniques for the treatment of hiatal hernias, but the most common are the Toupet and Nissen techniques. In both cases, after reducing the hernia in the abdomen and recalibrating the esophageal hiatus to the correct dimensions, the upper portion of the stomach is used to surround the distal portion of the esophagus (like a scarf).
By doing this, a valve is made that prevents acid reflux from rising into the esophagus.
The difference between the two procedures is that, in the case of a Toupet, the stomach is positioned to wrap around the esophagus by 180-270 degrees; while for the Nissen, the esophagus is encircled over 360 degrees.
The results are comparable for the two techniques, scientific studies have failed to show a difference between the two techniques at this level.
There is no difference, either, in complication rates, which is on average 5% and depends on the age of the patient (2% if under 50).
The Toupet procedure is preferable to the Nissen, however, because the most frequent type of complication after this second technique is difficulty eating (dysphagia), while, after Toupet, the most frequent complication is the recurrence of the reflux, which is less serious for the patient and does not require emergency treatment as in the case of dysphagia.
Instagram: To see videos/reels regarding robotic hernia surgery performed by Dr. Randone click on the icon in the bar of your screen or here.
Also see: INTERNATIONAL PATIENTS WELCOME
♦ To make an appointment with Dr. Bruto RANDONE, ENGLISH SPEAKING Digestive Visceral and Abdominal Surgeon, at the Clinique Internationale du Parc Monceau, 21 Rue de Chazelles, 75017 Paris, France, or at the Clinique Bizet, 22 bis Rue Georges Bizet, 75116 Paris, France, click on Contact.